National Accreditation Board for
Hospitals & Healthcare Providers
(NABH) CERTIFIED Institute

About
Mehta International Eye Institute
Mehta International Eye Institute is a recognized center for patient care, vision research and physician education our state-of-the-art facility is oriented towards providing patient-friendly care.
Our internationally renowned physicians possess the clinical and surgical expertise to provide consultations and medical-surgical care for complex ophthalmic problems.
Mehta International Eye Institute strives to maintain the most & up-to-date facilities so patients receive the best care possible. Mehta International Eye Institute has an eye care team that provides the professional support necessary to ensure that every patient receives personal attention. Our dedicated staff is highly trained in the art of patient care and draws on their many years of collective experience in assisting you.






Prof. (Dr.) Keiki R. Mehta
M.B.B.S., D.O.M.S., M.S. (OPHTH.), D.O. (IRELAND)
D.O. (LONDON), F.N.E.R.F. (U.S.A.)
F.R.S.H. (LONDON), F.I.O.S. (U.S.A.), FAICO.
Consultant Ophthalmic Surgeon, Medical Director & Chief
Awarded PADMASHREE by President of India
MEET THE DOCTOR
THE MOST QUALIFIED, SKILLFUL AND PROFESSIONAL DOCTOR
Dr. Keiki. R. Mehta, the surgical chief and director of Mehta International Eye Institute, graduated from Christian Medical College and completed his post-graduation.

Email
drkeiki@mehtaeyeinstitute.com

Emergency (24x7)
+91 98200 31041
+91 98197 60702
+91 98920 68684

Monday to Saturday : 10:00 AM - 09:00 PM
Sunday: Closed
Call to book an Appointment to meet us
FAQ's
Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon
Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon
Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon
Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon
Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon Text Coming soon


Our Work
Our Patients
Before & After Gallery
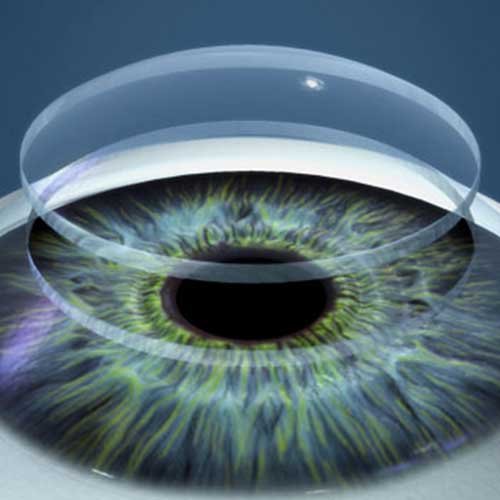
Mehta International Eye Institute (MIEI) has the most advanced, comprehensive list of equipment, making it the formost center for Ophthalmology in Asia and offers the entire range of eye treatments.
Make An Appointment
WE ARE SERVING PEOPLE FOR OVER 46 YEARS
BOOK AN APPOINTMENT

Our Quality Policy
We at Mehta International Eye Institute will provide the best quality of loving and caring humane services to our patients through our committed, professionally oriented team. We aspire for total customer Satisfaction in all ophthalmological services we undertake and will constantly strive for continual improvement.

Mission
We want you to see as well many years from now as you do today, so we spend extra time conducting a variety of tests you may not have experienced elsewhere.

Vision
Mehta International Eye Institute strives to maintain the most & up-to-date facilities so patients receive the best care possible.